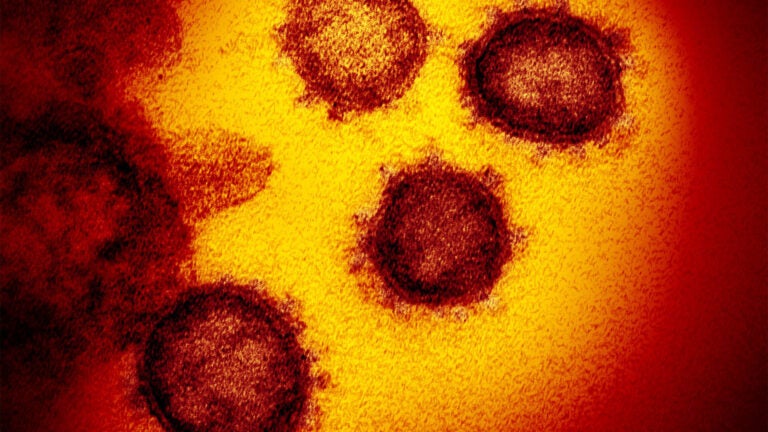
How close is ‘close’? What you need to know about COVID-19
USC Student Health answers the most commonly asked questions about the novel coronavirus, and what you can do to minimize your risk of exposure.
The present picture on COVID-19 is that it spreads through respiratory droplets — a sneeze, cough or other tiny watery fluid that gets expelled from one person and ends up in the eyes, nose or mouth of another person (sometimes carried by the hands as a go-between).
For most people in the U.S., the immediate health risk from COVID-19 is considered low because they are unlikely to have had an exposure. Health care workers caring for patients are at higher risk because they come into close contact with many patients and have more frequent potential exposures to biohazardous materials. (The total package of prevention gear, or “personal protective equipment” includes a gown, a tightly fitted nose/mouth mask, eye covering and gloves; sometimes the gown is swapped for ease of use with the full Tyvek “bunny suit” favored by electrical engineers in clean rooms). In the event of confirmed community spread (when the source of infection is not known or traceable) the risks to the public are elevated because, at that point, infection is no longer limited to identifiable points of contact.
So who would be at greater risk of having an exposure to COVID-19, and what might help stop the spread? The following definitions may help you understand the risks and potential planning landscape for future measures.
What is close contact?
Household members, intimate partners and caregivers in a non-health care setting may have “close contact” exposure (being within approximately 6 feet of a COVID-19 case for a prolonged period of time) if a person has an infection. When someone in the same household has an infection, the other members of the household should stay in another room or be separated from the patient as much as possible. Household members should use a separate bedroom and bathroom, if available.
In the event of a potential COVID-19 case in a shared living arrangement among USC students, the person who requires self-isolation would be temporarily moved to a single-occupancy living space for the duration of the isolation period, currently recommended as 14 days. The space would be thoroughly cleaned with a heightened protocol before returning to residential use. Fortunately, coronaviruses are vulnerable to all household disinfectants.
What is casual contact?
Casual contact is encountering an individual in a limited duration, typically in public space setting like a restaurant, library or outdoor space, where exchange of bodily fluids is unlikely.
What is the difference between self-isolation, quarantine and social distancing?
These three terms are related, but different descriptions for using space and time to slow transmission of infection in the general population:
Self-isolation is a voluntary adherence to a medical recommendation. The patient stays at home, avoids unnecessary contact with others and follows instructions for self-monitoring of symptoms, with follow-up by medical providers and/or public health officials.
Quarantine for individuals who may become sick (or isolation, for individuals who are already sick) involves a restriction of movement in order to slow the transmission of disease. Both quarantine and isolation are enforceable by agencies (local, state and federal public health officials) in order to protect the broader public. Yes, you can be compelled to stay in quarantine or isolation by public health authorities (not a medical provider).
Social distancing is a public health strategy to slow the progress of an epidemic so that structural areas of response — hospitals, emergency responders, health care settings, vaccine development and/or deployment — can have time to work with the most vulnerable to recover from illness and slow down further spread of illness in a community. Examples of social distancing measures include closing schools, cancelling large group gatherings and events, closing theaters, suspending worship services, etc. In the event of an epidemic, moving “in person” classes and business processes to “distance or web-based” operations help alleviate strain on the health care system by reducing person-to-person contact transmission.
Who is most at risk?
From the data that is currently available, it seems that older people, and people with underlying health conditions are most vulnerable to severe symptoms of COVID-19. The mortality rate climbs steadily with each age group. Many people who get COVID-19 have had mild symptoms and recovered; in the mildest cases, some people may not even have known they were infected, so the total infection rate is difficult to know. An individual with COVID-19 may be feeling relatively fine but can infect a more vulnerable older person who will come down with much more serious illness and additional medical complications.
So keeping our community safer through prevention and precautions (“keep calm and wash your hands”; non-contact greetings like “fight on!” instead of handshakes; staying home when you are sick) is the current best measure for keeping our most vulnerable members from harm, until an effective vaccine can be developed.
[info id=”24d7976f-25b2-4811-83d0-e614103cae1c” prefix=”7xz” format=”interactive” title=”Coronavirus cases”]