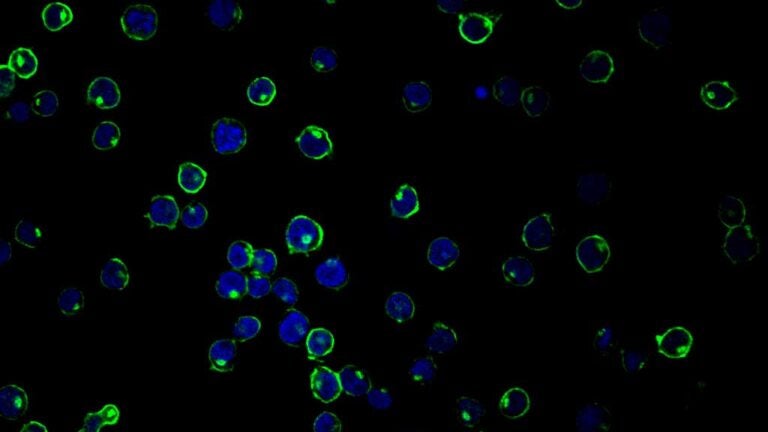
Delta 20 (green), a protein that suppresses HIV viruses, is highly expressed in HIV target cells that restrict acute HIV infection. Cell nuclei are shown in blue. (Image/Wan-Lin Wu)
USC researcher identifies a new potential way to treat HIV
Targeting human proteins may be a more effective treatment than using “HIV cocktails” to maintain health
Medical treatment that boosts the immune system rather than attacking ever-mutating viruses may one day help HIV-positive people whose bodies have built a resistance to anti-HIV cocktails, according to a Keck School of Medicine of USC researcher.
I-Chueh Huang has spent 13 years researching how the human immune system controls viral infections. His lab recently pinpointed a variant of a protein — one naturally found in the body — that helps fight HIV.
The study, published in the July 3 issue of the Proceedings of the National Academy of Sciences, is a first step toward enabling doctors to direct the body’s own immune system to better fend off disease.
So-called HIV cocktails, or highly active antiretroviral therapy (dubbed HAART), have enabled countless people with HIV to keep their viral counts low and keep HIV from progressing to AIDS. About 37 million people worldwide have HIV and 20 million received antiviral therapy in 2016, according to the World Health Organization.
Although most people are doing well with HIV-suppressing treatment, HIV eventually grows resistant to current drugs among many patients. That’s where Huang’s possible approach comes in.
“Most HIV drugs target the virus,” said Huang, assistant professor of molecular microbiology and immunology at the Keck School of Medicine. “But the virus is not stable; it always mutates — problematic because the virus can become resistant to effective drugs.”
Preventing viral spread
This new strategy builds on prior work from Huang’s lab. The researchers discovered that a family of proteins can restrict certain highly contagious viruses from reproducing themselves during early stages of infection. These viruses include SARS, influenza, dengue and West Nile.
The new study focused on HIV-1, the most widespread type of HIV worldwide.
HIV can be classified into R5 and X4 virus strains. R5 viruses are exclusively associated with primary infection, while X4 viruses emerge in later stages of HIV disease among half of HIV carriers. When doctors detect the X4 strain in a patient, it’s a sign that the patient’s HIV infection has progressed to a serious stage.
The Huang Lab found a way to suppress X4. Within the family of virus-stunting proteins they previously identified, they found that one particular protein could prevent the virus from infecting cells. They nicknamed it “Delta 20.”
Huang and his colleagues hope the research leads to new strategies besides vaccination to stoke the immune system to fight HIV.
“Our finding will not help develop a vaccine because the focus is on innate immunity rather than the virus,” Huang said. “Perhaps one day scientists will create medicine that, like ‘HIV cocktails,’ have to be taken indefinitely. But the new treatment may be more effective because it is harder for viruses to escape the body’s defenses.”
Researchers across disciplines at USC are working on several strategies to attack HIV and other viruses. For example, Paula Cannon at USC Stem Cell is working to edit human genes to create HIV-resistant cells.
The study was supported by the National Institutes of Health (P30 DK048522) and the National Institute of Allergy and Infectious Diseases (R01AI100953).
