
Rebecca Trotzky-Sirr is fighting the opioid epidemic one patient at a time. (Photo/ Gregg Segal)
The USC Experts on the Front Lines of the Opioid Epidemic
Nearly 400,000 people in America died from opioid overdose from 1999-2017. USC experts believe they can stem the tide.
The doors to the emergency room swung open, and in walked Samuel.
Again.
The doctors and nurses in the emergency room at Los Angeles County+USC Medical Center knew him too well. They also knew his desperation. He wanted more painkillers.
After a football injury in high school, Samuel had grown addicted to prescription pain pills. By his early 20s, he had moved on to heroin and ended up living on the street.
On his first few visits to the ER, he was agitated and antsy, and often tried to fight with the staff.
And he asked the same angry question time after time. “Why aren’t you giving me my pain medicine?”
It’s a story that plays out regularly in doctors’ office and clinics from rural America to big cities. Like ER doctors across the U.S., LAC+USC emergency physician Rebecca Trotzky-Sirr sees patients like Samuel every day — patients hooked on the euphoric, calming qualities of opioid drugs.
“There’s a big, not-surprising overlap between people who are experiencing a trauma or emergency who also are intoxicated or have a problem with substance abuse,” says Trotzky-Sirr, medical director of the LAC+USC Urgent Care Center. “The opioid crisis has made it even more common.”
Hundreds of thousands of people like Samuel live from dose to dose of opioids, whether they’re prescription tablets or injected heroin.
And scores are losing their lives.
Every day, 130 people die from opioid overdoses, according to a 2017 report by the Centers for Disease Control and Prevention. It’s the worst drug epidemic in U.S. history, prompting the federal government to declare it a national emergency.
In 2017, the U.S. Department of Health and Human Services declared the widespread abuse of opioid medications a public health emergency.
State and national leaders are scrambling to get a handle on the epidemic. USC faculty and health administrators are part of a national mobilization of experts who are tackling the crisis on several fronts. They’re seeking better ways to treat pain and control the administration of opioids, dissecting the science of addiction and searching for less-addictive medicines.
A Crisis Decades in the Making
The opioid epidemic blew up in three distinct waves, according to medical experts and sociologists.
The first wave of opioid-related deaths goes back to the 1990s, when medications such as oxycodone were aggressively marketed to physicians with assurances that they posed a low risk of addiction —promises that proved wrong.
A second wave, beginning around 2010, resulted from growing heroin use. People who had become addicted to painkillers turned to heroin because it was cheaper and easier to get than prescription medicine.
The third wave began in 2013, when overdose deaths due to synthetic opioids spiked sharply. These drugs include illicitly manufactured fentanyl. It’s similar to morphine but 50 to 100 times more potent.
By the time the nation awoke to the burgeoning crisis, a lot of damage had been done.
Now health professionals, researchers and first responders are “just trying to figure out how to get everyone the help they need and stop people from dying,” says pain management expert Melissa Durham, an associate professor of clinical pharmacy at the USC School of Pharmacy.
Sociologist Ricky Bluthenthal says that one of the reasons the opioid crisis exploded is because the painkillers are so readily available.
“Some illicit drugs are geographically specific, but opioids are almost everywhere, regardless of where you live,” says Bluthenthal, a professor of preventive medicine and drug epidemiologist whose work on the effects of drug injections dates back to the AIDS epidemic in the early 1990s. “This national component really distinguishes the opiate crisis from any other drug crisis that has happened.”
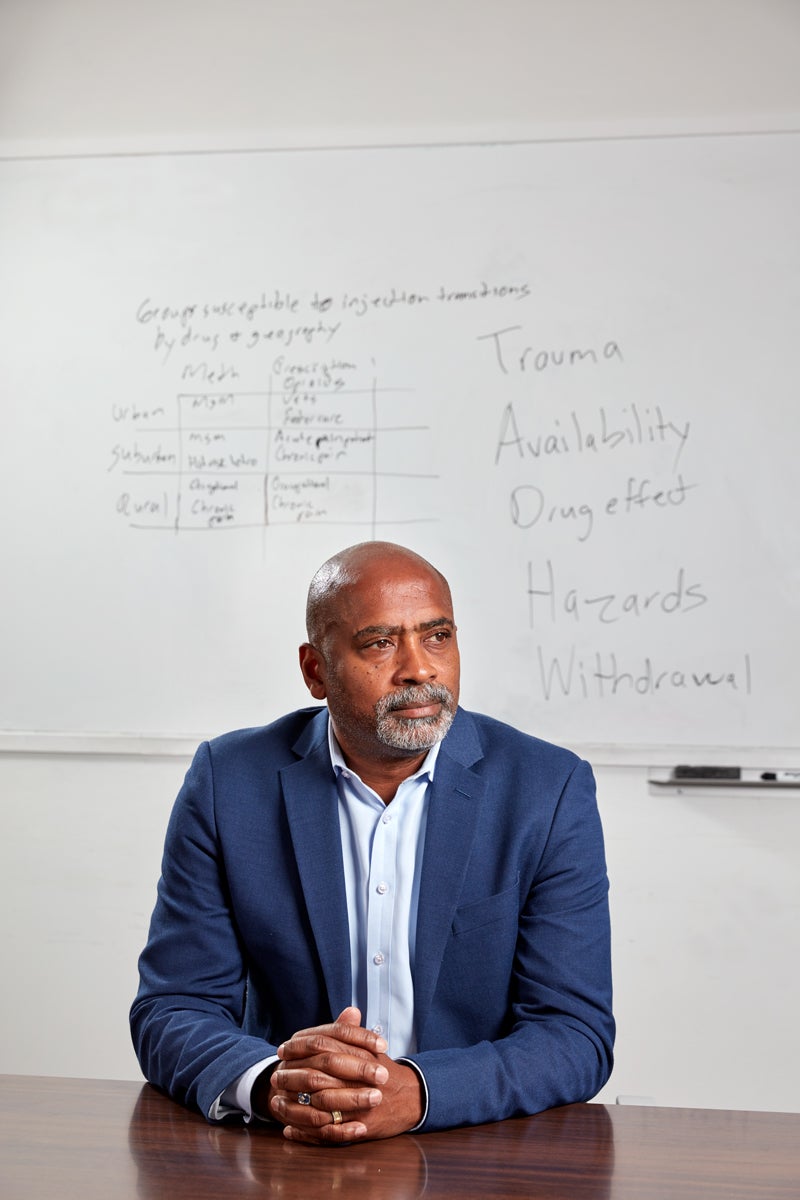
Another devastating distinction, Bluthenthal adds, is that addicts are in it for the long haul. Unlike methamphetamine, which addicts typically burn out on after five to six years, opioids often lead to a chronic, decades-long addiction.
USC Opioid Experts’ Recommendation: Prescribe Carefully
Durham established a pharmacist-run pain medication management clinic at the USC Pain Center in 2008, during a time when opioids were widely viewed as a standard option to treat chronic pain. Previously, prescribers mostly restricted these medications to patients with cancer or those recovering from surgery.
Today, the practice of prescribing opioids as the “go-to” therapy for chronic pain is changing in response to the crisis, Durham says.
U.S. prescribers also have clamped down on opioid prescriptions. They wrote 22 percent fewer in 2017 than in 2013. And anyone who writes an opioid prescription now must check a state tracking database.
At Keck Medicine of USC, health professionals are following new guidelines for prescribing opioids. They aim to reduce risk and improve patient care. And for surgical patients, Keck Medicine has introduced an initiative to reduce and even avoid opioid use. It’s called enhanced recovery after surgery, or ERAS. Led at USC by anesthesiologists Michael Kim and Carol Peden, ERAS shows promise. Some surgical groups have cut their opioid prescriptions by 75% in only six months. Patients were less likely to have complications after surgery or be readmitted to the hospital. They’ve also been able to leave the hospital faster.
More than 130 Americans die every day from opioid-related overdoses.
Being more careful about how and when opioids are prescribed is also a big concern for Lorraine Kelley-Quon, a pediatric surgeon at USC-affiliated Children’s Hospital Los Angeles. She operates on young patients, whether they’re premature babies in emergency surgery or teens involved in car crashes. So she understands that children in pain have unique needs. She is working with the American Pediatric Surgical Association to create guidelines for prescribing opioids for children after surgery.
“If you look at the research literature, you could say that in the past few years, surgeons kind of woke up and said, ‘Hey, we’re giving too many opioids after surgery. Maybe we can minimize that,’” she explains.
Patients might have certain characteristics that physicians should consider when deciding whether to prescribe them opioids, and for how long, Kelley-Quon says. She is evaluating how behavioral health conditions may be tied to patients’ risk for opioid addiction after surgery. These include issues like anxiety, depression and ADHD.
“Doctors could say, ‘I have this kid with anxiety, I need to be very judicious about giving him opioids,’” she explains.
Yan Liu, a USC Viterbi School of Engineering associate professor in computer science, is working on stopping opioid addiction before it begins. It’s a surprising project considering she’s an expert in artificial intelligence.
Applying sophisticated mathematical models to the electronic medical records of 150,000 patients at the Mayo Clinic in Rochester, Minnesota, Liu aims to sift through data to identify which patients are more likely to develop an addiction to opioid-based pain medication.
The computer program would look for characteristics shared by people who are vulnerable to becoming addicted to opioids, giving doctors an important red flag before opioids are prescribed. And some scientists are developing genetic tests that can predict who’s likely to become addicted.
One promising strategy to reduce opioid prescriptions focuses on ordinary doctors’ offices, where many of these prescriptions are written for routine pain.
In one study, Jason Doctor, a behavioral economist at the USC Leonard D. Schaeffer Center for Health Policy & Economics, and Jonathan Lucas, chief medical examiner-coroner for Los Angeles County, found that doctors decreased opioid prescriptions by nearly 10 percent after being informed that a patient in their care had fatally overdosed. Doctor and Lucas examined a year of opioid-related deaths in San Diego County.
Nearly 80% of heroin users reported misusing prescription opioids prior to heroin.
During that time, more than 860 doctors had prescribed opioids to 170 patients who later overdosed. San Diego County’s chief medical examiner subsequently sent a carefully worded letter to each physician that was supportive, not accusatory, in tone. In response, the physicians wrote fewer opioid prescriptions.
“Doctors need to know what’s happened to their patients, and that someone is paying attention, so they can help avoid deaths while they seek to alleviate pain,” Doctor and Lucas wrote in an opinion piece published in USA Today.
The Need for Relief and Roots of Addiction
“This is the first time we’ve really had a drug-use epidemic that has started through the health care system,” says Bluthenthal, the drug epidemiologist. Concern about opioid addiction has curbed the availability of prescriptions so much that it has spurred a backlash. Some chronic pain patients who legitimately relied on the medicines find it difficult to get them anymore. Health experts acknowledge the difficulty of balancing the risk of addiction with their responsibility to be humane and ease pain.
This balancing act only underscores the need for USC researchers to develop alternative medications to ease pain. Across the world, scientists are on a quest to find drugs that work differently.
Last year, scientists from the Bridge Institute at the USC Michelson Center for Convergent Bioscience and colleagues made a major breakthrough toward new non-addictive medications. They discovered an opioid-based compound that activates a specific receptor tied to pain relief — but doesn’t activate receptors linked to opioids’ dangerous side effects. Such medicines would go straight to the site of pain, detouring the pleasure reward centers in the brain that spawn euphoria and drive people toward addiction.
“That’s the holy grail: coming up with a new medication that’s going to treat pain without getting people addicted,” says Adam Leventhal, professor of preventive medicine and psychology and director of the USC Health, Emotion and Addiction Lab.

Experts know that finding better painkillers won’t fix the problem on its own. They also have to understand more about what causes addiction. That’s why USC has recognized and funded a growing collaboration on addiction science led by Leventhal. It involves experts across USC, from pharmacy scientists to social workers. They’re starting new research projects and educational initiatives centering on addiction issues, including the opioid epidemic.
Humanity has a long history of addiction, Leventhal says, and society has gotten more sophisticated in getting people hooked on the next big thing.
“Opioids are part of a larger addiction crisis,” he says. “You’ve got new forms of commercialized cannabis, a youth nicotine vaping epidemic, and a whole generation addicted to their smartphones.”
Leventhal says the differences in how individual brains are wired can vary drugs’ addictive qualities from person to person. “For some, opioids can produce pain relief without much euphoria,” he says. “For others, opioids produce powerful euphoria and a sense of calm that can be difficult to cultivate naturally.”
Once addicted, many need medical help to break free.
Road to Recovery from Opioid Addiction
Health professionals have a variety of medications they can prescribe — in combination with counseling, physical therapy and occupational therapy — to try to wean patients off opioids. Prescribers are turning to low-dose naltrexone, an opioid receptor antagonist that is used to save people in the throes of an opioid overdose. And emergency medicine doctors like Trotzky-Sirr increasingly use buprenorphine, which reduces withdrawal symptoms when patients stop using opioids.
Treating substance abuse disorders has become a critical part of care at LAC+USC, Trotzky-Sirr says. The concept, still evolving, involves ER doctors seeing substance abuse disorders as diagnosable and treatable diseases. In the past, she says, ER doctors simply would refer patients to their primary care doctors for this type of care. But recent research suggests that patients who start their treatment for opioid abuse in the emergency room have a greater chance of sticking with their treatment.
For patients like Samuel, the former athlete treated by Trotzky-Sirr at LAC+USC, the emergency room became his doorway to sobriety.
His physicians gave him buprenorphine, which eased him off the grinding ups and downs of addiction. Within the first month after quitting heroin, he reconnected with his family.
In the second month, he showed up at an appointment with Trotzky-Sirr wearing a three-piece suit for a job interview scheduled for later that day.
“He was one of the most dapper patients I’ve ever seen,” she recalls.
Today, Samuel has a job, stable housing and a steady girlfriend. Trotzky-Sirr hopes the words he told her will become routinely heard at LAC+USC’s Urgent Care Center and in emergency rooms everywhere:
“Thank you so much for saving my life. I feel like my old self.”



