The USC Stem Cell laboratory of Andy McMahon has identified a type of injured cell that might contribute to the transition from an acute kidney injury to chronic kidney disease, as described in a new study published in the Proceedings of the National Academy of Sciences (PNAS). The same issue of PNAS also features an accompanying Q&A with McMahon to mark his recent election as a member of the National Academy of Sciences.
“Acute kidney injury can be a common side effect of surgery, sepsis or certain prescription drugs, and there is no effective treatment,” said McMahon, who is the W.M. Keck Provost and University Professor of Stem Cell Biology and Regenerative Medicine, and Biological Sciences at USC. “Even a mild or moderate injury can progress into chronic kidney disease, which affects 9.1 percent of the world’s population and causes 1.2 million deaths each year.”
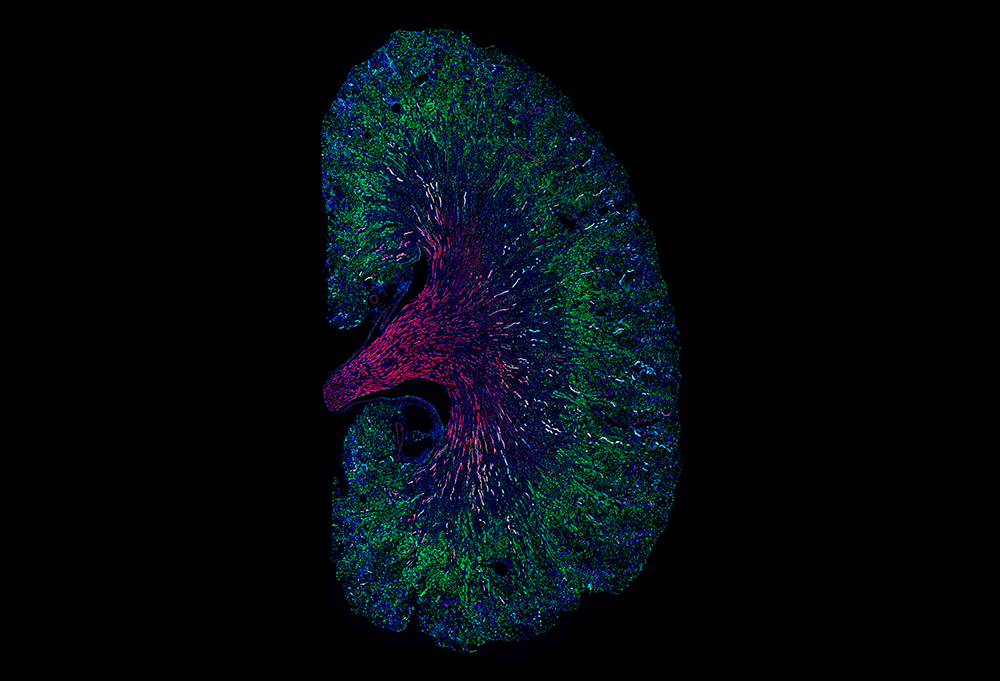
The adult kidney lacks stem cells to regenerate damaged tissue in its approximately 1 million filtering units, which are called nephrons. Damage predominantly occurs in a segment of the nephron known as the proximal tubule. Fortunately, differentiated proximal tubule cells (PTCs) do have their own capacity to repair.
To understand this repair process, first authors Louisa M. S. Gerhardt, Jing Liu, and their colleagues in the McMahon Lab pioneered a way to track injured PTCs in lab mice by using a protein called keratin-20, which the cells tend to produce after acute kidney injury.
As expected, when a sudden injury provoked the death of some PTCs, surviving ones multiplied to repair the injury. However, weeks after kidney function was restored, the scientists observed that PTCs, which failed to repair normally, appeared at the site of the original injury, and also in regions remote from the initial injury. Unlike normal PTCs, these damaged cells showed activity of gene networks implicated in inflammation, scarring, and cell migration— features associated with a slow progression to chronic kidney disease.
Some of the harmful PTCs showed activity in both genes that support survival and genes that promote programmed cell death, the normal process through which irreparably damaged cells self-destruct. As is observed in cancers, pro-survival genes may prevent programmed cell death, despite abnormalities that would normally limit cell survival, making it more likely for damaged cells to linger, promoting disease progression.
“This research presents a dynamic picture of how the initial injury, even if mild, leads to the creation of harmful PTCs that likely contribute to chronic kidney disease,” said McMahon, who is also the Director of the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC. “Our study also raises the possibility of targeting these harmful PTCs for destruction, either by priming them for immune attack or by removing the genes that are interfering with the normal safeguard of programmed cell death.”
Additional co-authors of the study include Kari Koppitch and Pietro E. Cippa in the McMahon Lab.
Fifty percent of this work was supported by U.S. federal funding from the National Institute of Diabetes and Digestive and Kidney Diseases to the (Re)Building a Kidney consortium (partnership grant U01DK107350 and program grant UC2DK126024). The remainder of the funding came from the German Research Foundation (postdoctoral scholarship GE 3179/1-1), Swiss National Science Foundation (grant 167773), Gianella Foundation and Balli Foundation.
